Vascular surgery is a specialty of surgery in which diseases of the vascular system, or arteries and veins, are managed by medical therapy, minimally-invasive catheter procedures, and surgical reconstruction.
Surgery for Blocked Arteries
What is Embolectomy?
What is embolus or embolism?
Emboli are abnormal masses of material (which can be solid, liquid or gas) that are carried in the blood stream from one part of the circulation to another causing a blockage (occlusion) of a blood vessel that leads to lack of oxygen supply (ischemia) and finally death of tissue downstream of the embolus.
The most common type of emboli are a blood clot generated by thrombosis in the left side of the heart mostly due to valvular heart disease, which then breaks off and is then transported in the blood stream.
In other cases the atherosclerotic plaque in major or smaller arteries may get eroded and a clot is formed on the spot.
What are the treatment options:
Indications :
Embolectomies are performed for arterial embolisms in acute limb ischemia. This procedure can be done under local anesthesia , and mostly general anesthesia is not required.
catheter-directed thrombolysis and anticoagulation with observation.(but these options are applicable when the patient appears in time, means 8 to 12 hrs from the time of onset of severe acute pain symptoms). It can also be used for other ischemias due to embolism for example mesenteric ischemia and stroke.
Cathater directed Thrombolysis :
In the diseased artery a multiperforated catheter is inserted and through that catheter thrombus or clot lysing medicines are infused continuously for 24 -48 hours . this gradually lyses the clot and the artery opens up.
This technique is good when the patient reaches to the centre in less than 12 hrs, as the clot is soft so lyses easily.
This prevents sudden gush of blood flow to the diseased segment hence sudden release of toxins to the body circulation does not happen so is well tolerated specially in younger patients.
Balloon embolectomy :
Typically this is done by inserting a catheter with an inflatable balloon attached to its tip into an artery, passing the catheter tip beyond the clot, inflating the balloon, and removing the clot by withdrawing the catheter. The catheter is called Fogarty, named after its inventor Thomas J. Fogarty.
Possible complications of balloon embolectomy include intimal lesions, which can lead to another thrombosis. The vessel may also be affected by dissection or rupture.
Aspiration Embolectomy :
Here the thrombus is removed by suction rather than pushing with a balloon. It is a rapid and effective way of removing thrombi in thromboembolic occlusions of the limb arteries below the inguinal ligament, as in leg infarction.
Surgical Embolectomy :
Surgical embolectomy is the simple surgical removal of a clot following incision into a vessel by open surgery on the artery this is used for visceral embolectomies eg. Mesentric thrombosis, pulmonary artery thrombosis.
Outcome
Outcome of embolectomy varies with size and location of the embolus. Embolectomy when done in time ( < 12 hrs) has excellent results, but when it is delayed the outcome is uncertain and even may be due to the deleterious effects of toxins released in the blood circulation (Reperfusion injury) from the dying muscles and organs may even turn life threatening.
So always timely referral and timely intervention is the key to success.
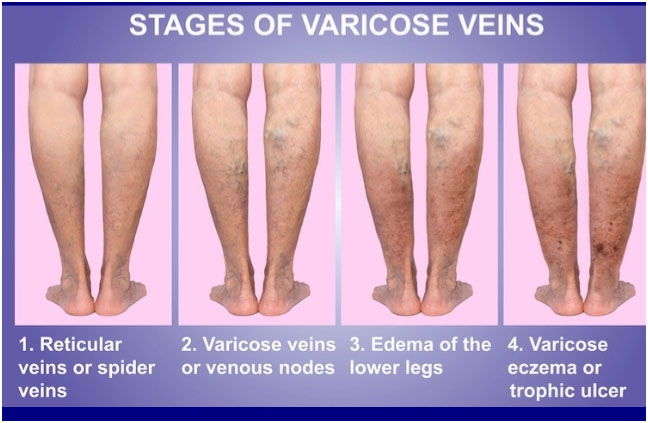
Varicose Veins
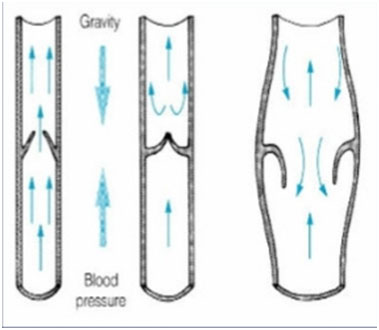
Blood circulates from the heart to the legs via arteries and back to the heart through veins. Veins contain one-way valves which allow blood to return from the legs against gravity. If the valves leak, blood pools in leg veins which can become enlarged or varicose.
These dilated veins keep engorged and thus cause swelling of the leg mostly by the evening and the leg aches in evening and night. Once the night rest is taken the swelling disappears and the pain subsides and again when the person starts working the same cycle starts again.
Varicose Veins Treatment
Endovenous ablation techniques use radiofrequency or laser energy to cauterize and close varicose veins in the legs.
Varicose vein stripping in which surgically the diseased vein is removed.
Endovenous Ablation of Varicose Veins
Endovenous ablation, is a minimally invasive treatment that uses radiofrequency or laser energy to cauterize (burn) and close abnormally enlarged veins in the legs.
Using ultrasound to visualize the enlarged vein, a catheter or vascular access sheath is inserted through the skin and positioned within the abnormal vein. A laser fiber or radiofrequency electrode is then inserted through the catheter and advanced to the desired location. Laser or radiofrequency energy is then applied, heating the vessel and causing it to close. Following the procedure, the faulty vein will shrink and "scar down."
After the procedure?
Following the procedure, you will need to wear a gradient compression stocking to help reduce bruising, tenderness, and minimize the rare possibility that blood clots may form.
Some patients specially females may experience pain after procedure for a week or so, such patients may need some pain killers for a week.
You may resume your normal activity immediately, with the exception of air travel or prolonged sitting (such as a long car trip). You should remain active and not spend too much time in bed during the recovery period since this increases the chance of complications.
Who interprets the results and how do you get them?
A follow up ultrasound examination is essential in order to assess the treated vein and to check for adverse outcomes. Within one week, the target vein should be successfully closed. Additional procedures (such as sclerotherapy or phlebectomy) may be necessary to treat associated veins.
What are the benefits vs. risks?
Benefits
No surgical incision is needed—only a small nick in the skin that does not have to be stitched closed.
When compared with traditional vein stripping techniques, endovenous ablation is more effective, has fewer complications, and is associated with much less pain during recovery.
Endovenous ablation is generally complication-free and safe.
This procedure leaves virtually no scars because catheter placement requires skin openings of only a few millimeters, not large incisions.
Endovenous ablation offers a less invasive alternative to standard surgery.
Most of the veins treated are effectively invisible even to ultrasound 12 months after the procedure.
Most patients report symptom relief and are able to return to normal daily activities immediately, with little or no pain.
What are the limitations of Endovenous Ablation of Varicose Veins?
Ablation catheters cannot be easily passed through a tortuous vein, or a vessel with many turns and bends. Consequently, the procedure is typically used to treat larger varicose veins, such as the great saphenous vein, which extends from the groin down the inside of the thigh into the inner calf.
Endovenous ablation is successful at closing the abnormal target vein almost 100 percent of the time, but small dilated branches that persist in the skin often require additional treatment with phlebectomy (minor surgical procedure to extract them) orsclerotherapy (injection of a liquid medication to seal them off). Subsequent treatments are usually scheduled after an ablation procedure.
Surgical stripping of Varicose veins
In this operation the surgeon after giving spinal anesthesia (Anesthesia which makes the lower body numb by giving injection in spine) makes 2 small incisions, one in the lower leg and another in the upper thigh. The incisions are approx 1 – 2 inch long. The varicose vein is identified and a small wire is passed from the one end of vein and received from other end. The vein is tied to the wire and then the wire is pulled hardly to remove the vein . this procedure removes the vein by avulsing it completely.
Immediately after the operation after the incision is repaired the stockings or crepe bandage is applied to control the internal bleeding.
Postoperative skin discoloration and swelling and pain are usual side effects of surgery. But they gradually disappear with time and painkiller tablets.
Patient usually can get discharge by next day or 2.
Benefits
Drawbacks
My Recommendations :
I personally recommend endovenous laser ablation to patients who have symptomatic varicose veins, (which is radiologically severe). In most of cases I personally ligate the junction by a 5 mm incision and then ablate the GSV, this leads to better results and lesser laser energy.
Surgical stripping is mostly for those who have financial constraints or are relapsed after previous endovenous ablations.
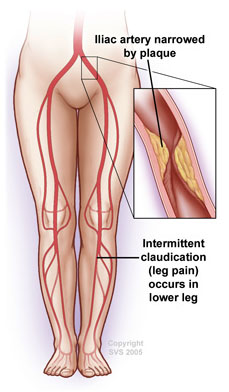
Aortoiliac Occlusive Disease
What is aortoiliac occlusive disease?
Aortoiliac occlusive disease occurs when your iliac arteries become narrowed or blocked. The aorta, your body's main blood pipe, splits into branches at about the level of your belly button. These branches are called the iliac arteries. The iliac arteries go through your pelvis into your legs, where they divide into many smaller arteries that run down to your toes.
Your arteries are normally smooth and unobstructed on the inside, but as you age, a sticky substance called plaque can build up in the walls of your arteries. Plaque is made up of cholesterol, calcium, and fibrous tissue. As more plaque builds up, it causes your arteries to narrow and stiffen. This process is called atherosclerosis, or hardening of the arteries. Eventually, enough plaque builds up to interfere with blood flow in your iliac arteries or leg arteries. Physicians call this aortoiliac occlusive disease because it involves the aortoiliac arteries.
When your iliac arteries narrow or become blocked, your legs may not receive the blood and oxygen they need. This lack of oxygen is called ischemia and it can cause pain. In severe cases, sores or gangrene can develop, which can result in losing a limb. However, these developments are uncommon unless the process is not treated and is allowed to progress.
What are the symptoms?
Early in the disease, you may feel pain, cramping, or fatigue in your lower body when you walk or exercise. The pain with walking usually occurs in your buttocks, thighs, and legs. This symptom is called intermittent claudication because it stops when you rest. As the disease worsens, you may find that pain occurs when you walk for shorter distances. Ultimately, as the disease progresses, you may feel pain, usually in your toes or feet, even when you are resting.
Some men who have aortoiliac occlusive disease also experience erectile dysfunction, the inability to have or maintain an erection.
Aortoiliac disease may worsen if it is not treated. Signs that it has advanced include:
If you experience any of these advanced symptoms, it usually means that your leg arteries are blocked in more than one place. Your physician may need to treat more than one site to prevent gangrene or limb loss.
What causes aortoiliac occlusive disease?
In rare cases, a condition known as Takayasu’s arteritis may cause blockages in your aorta and its branches. Takayasu’s arteritis usually affects young Asian women between the ages of 10 and 30. It is caused by inflammation in the arteries.
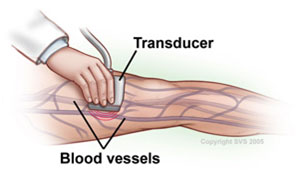
Doppler Ultrasound
Doppler ultrasound is non-invasive test that diagnoses the presence or absence of blockage in the blood vessel. To certain extent it may diagnose the severity of blockage by indirect estimation. So it is the test to find out whether there is block or not.
Angiography
There are three types of arteriography that may be performed: contrast arteriography, CT angiography (CTA), and MR Angiography (MRA). Contrast arteriography usually provides better resolution but is a more invasive test. Your physician injects a contrast dye into your arteries and then takes x-ray images. The structure of your arteries appears on the x-ray pictures because x-rays themselves cannot pass through the dye. This test finds the exact location and pattern of blockages. The dye is later passed from your body through your kidneys.
How is aortoiliac occlusive disease treated?
Lifestyle Changes
Angioplasty or Surgery
If you have severe aortoiliac occlusive disease, particularly if it does not improve with the measures described above, your physician may recommend a minimally invasive treatment called angioplasty to improve the circulation in your legs. For more extensive blockages or those that cannot be treated with angioplasty, surgery to bypass or clear your blocked arteries may be required.
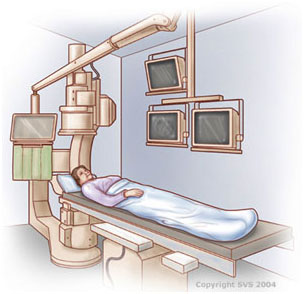
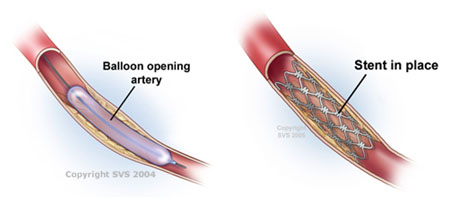
During an angioplasty procedure, which is sometimes performed at the same time as an angiogram, a long, thin, flexible tube, called a catheter, is inserted into a small puncture over an artery in your leg and is guided through your arteries to the blocked area. Once there, a special balloon attached to the catheter is inflated and deflated several times. The balloon pushes the plaque in your artery against your artery walls, widening the vessel. In some circumstances, a tiny mesh-metal tube called a stent may then be placed into the narrowed area of your artery to keep it open. The stent remains permanently in your artery. After successful angioplasty, blood flows more freely through your artery.
Bypass surgery, usually done through abdominal or leg incisions depending upon the location of the blockage, creates a detour around the narrowed or blocked sections of your artery. A Y-shaped tube made of synthetic fabric, called a graft, is attached to your aorta above the blockage. The two branches of the graft are then attached to either your left and right iliac arteries or other major arteries in each leg (called the femoral arteries). Although more invasive, bypass surgery restores blood flow in about 85 percent of patients. Results are commonly maintained for 10 or more years.
An endarterectomy is a way for your surgeon to remove the plaque from your artery. To perform an endarterectomy, your vascular surgeon makes an incision in your leg or abdomen, depending upon the location of the blockage in the artery, and removes the plaque contained in the inner lining of the diseased artery. This leaves a wide-open artery and restores blood flow through your leg artery.
The best choice of the treatment depends upon the pattern of blockage as well as how much blockage you have. Your vascular surgeon will help you determine which method of treatment is best for your particular situation.
Aortic Aneurysm
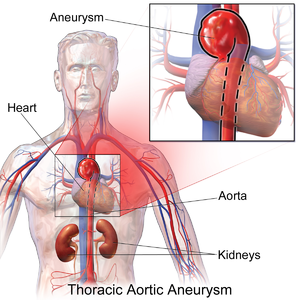
An aortic aneurysm is enlargement (dilation) of the aorta to greater than 1.5 times normal size. They usually cause no symptoms except when ruptured. Occasionally there may be abdominal, back or leg pain. They are most commonly located in the abdominal aorta, but can also be located in the thoracic aorta. Aortic aneurysms cause weakness in the wall of the aorta and increase the risk of aortic rupture. When rupture occurs, massive internal bleeding results and, unless treated immediately, shock and death can occur.
Signs and symptoms
Most intact aortic aneurysms do not produce symptoms. As they enlarge, symptoms such as abdominal painand back pain may develop. Compression of nerve roots may cause leg pain or numbness. Untreated, aneurysms tend to become progressively larger, although the rate of enlargement is unpredictable for any individual. Rarely, clotted blood which lines most aortic aneurysms can break off and result in an embolus. Medical imaging is necessary to confirm the diagnosis and to determine the anatomic extent of the aneurysm.
Aortic rupture
An aortic aneurysm can rupture from wall weakness. Aortic rupture is a surgical emergency, and has a high mortality even with prompt treatment.
Risk factors
Pathophysiology
An aortic aneurysm can occur as a result of trauma, infection, or,most commonly, from an intrinsic abnormality in the elastin and collagen components of the aortic wall.
Management
Surgery (open or endovascular) is the definite treatment of an aortic aneurysm. Medical therapy is typically reserved for smaller aneurysms or for elderly, frail patients where the risks of surgical repair exceed the risks of nonoperative therapy (observation alone).
Medical therapy
Medical therapy of aortic aneurysms involves strict blood pressure control. This does not treat the aortic aneurysm per se, but control of hypertension within tight blood pressure parameters may decrease the rate of expansion of the aneurysm.
The medical management of patients with aortic aneurysms, reserved for smaller aneurysms or frail patients, involves cessation of smoking, blood pressure control, use of statins and occasionally beta blockers. Ultrasound studies are obtained on a regular basis (i.e. every six or 12 months) to follow the size of the aneurysm.
Surgery
Decisions about repairing an aortic aneurysm are based on the balance between the risk of aneurysm rupture without treatment versus the risks of the treatment itself.
A rapidly expanding aneurysm should under normal circumstances be operated on as soon as feasible, as it has a greater chance of rupture. Slowly expanding aortic aneurysms may be followed by routine diagnostic testing (i.e.: CT scan or ultrasound imaging).
For abdominal aneurysms, the current treatment guidelines for abdominal aortic aneurysms suggest elective surgical repair when the diameter of the aneurysm is greater than 5 cm (2 in). However, recent data on patients aged 60–76 suggest medical management for abdominal aneurysms with a diameter of less than
Open Surgery
Open surgery typically involves exposure of the dilated portion of the aorta and insertion of a synthetic (Dacron or GoreTex) graft (tube). Once the graft is sewn into the proximal (toward the patient's head) and distal (toward the patient's foot) portions of the aorta, the aneurysmal sac is closed around the graft The aorta and its branching arteries are crossclamped during open surgery. This can lead to inadequate blood supply to the spinal cord, resulting in paraplegia, when repairing thoracic aneurysms. Cerebrospinal fluid drainage, when performed in experienced centers, reduces the risk of ischemic spinal cord injury by increasing the perfusion pressure to the spinal cord.
Endovascular
Endovascular treatment of aortic aneurysms is a minimally invasive alternative to open surgery repair. It involves placement of an endovascular stent through small incisions at the top of each leg into the aorta. As compared to open surgery, EVAR has a lower risk of death in the short term and a shorter hospital stay but may not always be an option.There does not appear to be a difference in longer term outcomes between the two. After EVAR, repeat procedures are more likely to be needed.
Peripheral Aneurysms
What are peripheral aneurysms?
Peripheral aneurysms affect the arteries other than the aorta. Most peripheral aneurysms occur in the popliteal artery, which runs down the back of your lower thigh and knee. Less commonly, peripheral aneurysms also develop in the femoral artery in your groin, the carotid artery in your neck, or sometimes the arteries in your arms.
If you have a peripheral aneurysm in one leg, you are more likely to have an aneurysm in the other leg. You also have a greater chance of having an aortic aneurysm.
Aortic aneurysms can cause serious complications because they can burst or rupture. Peripheral aneurysms do not rupture as often as aortic aneurysms, although they can do so. However, peripheral aneurysms more commonly can form clots that may block blood flow to your limbs or brain. Peripheral aneurysms, especially if they are large, can also compress a nearby nerve or vein and cause pain, numbness, or swelling.
What are the symptoms?
You may not feel symptoms with a peripheral aneurysm, especially if it is small. Two out of 3 patients with a peripheral aneurysm may not notice any symptoms. If you do have symptoms, the warning signs will depend on the location and size of your aneurysm. Possible symptoms include:
If the carotid artery is involved, the symptoms can include transient ischemic attacks (TIA) or stroke.
What causes peripheral aneurysms?
Peripheral aneurysms may be caused by infection or injury in unusual circumstances, but the actual cause of most peripheral aneurysms is not known with certainty. Researchers believe that atherosclerosis also called “hardening of the arteries” is associated with many peripheral aneurysms. Your arteries are normally smooth and unobstructed on the inside but, as you age, they can become blocked through atherosclerosis. In atherosclerosis, a sticky substance called plaque builds up in the walls of your arteries. Over time, your arteries narrow, stiffen, and possibly weaken. Factors that increase your risk for atherosclerosis include:
Your risk of developing peripheral aneurysms also increases as you age. People are usually in their 60s and 70s when they are found to have peripheral aneurysms. What tests will I need?
First your physician will usually ask questions about your general health, medical history, and symptoms. In addition, your physician conducts a physical examination. Together these events are known as a patient history and exam. As part of your history and exam, your physician may check for an aneurysm in your groin or thigh.
If your physician suspects you have a peripheral aneurysm, he or she may order an ultrasound or other imaging test, such as a computed tomography (CT) or magnetic resonance imaging (MRI) scan to confirm it. Angiography, which is more invasive, may be required in some circumstances to plan surgery or deliver medications if this is required.
It is known that many patients who have a peripheral aneurysm also have heart disease. Before performing surgery to treat your peripheral aneurysm, your physician may order tests to check on your heart, such as an electrocardiogram (ECG) or stress test.
How are peripheral aneurysms treated?
Your treatment will depend on the location of your aneurysm, the size of your aneurysm, your symptoms, and whether or not the aneurysm is completely blocked by clots at the time of its discovery. For example, if you have a popliteal aneurysm that is blocked and yet you are having no symptoms, you may not need surgery. In that situation, for example, your physician may recommend that you:
Vascular surgeons usually treat peripheral aneurysms with a surgical bypass or replacement. During this operation, your vascular surgeon constructs a new pathway for blood to flow by using a graft. A bypass graft may be made from a portion of one of your veins or sometimes a man-made tube, formed from plastic or other materials, that your surgeon connects above and below the aneurysm to allow blood to pass around it. If you need bypass surgery, you will receive regional or general anesthesia. Following the surgery, depending upon the location of your aneurysm, you may need to stay in the hospital for 2 to 7 days.
In some circumstances, if a peripheral aneurysm is blocked by a clot, medications known as thrombolytic agentsmay be used to dissolve the clots in preparation for bypass surgery. This procedure is sometimes done at the time of angiography, if needed.
The use of endovascular therapy, such as stent grafts, for the treatment of peripheral aneurysms is still in the investigational stages. Nevertheless, endovascular therapy may have a role in the treatment of some patients with peripheral aneurysms, especially if the risk for surgical repair is felt to be too high and the aneurysm has a favorable location and shape for an endovascular graft.
Very rarely, some patients with popliteal or femoral aneurysms may initially have a limb that is beyond saving because of extensive gangrene or infection or they may be too sick to undergo bypass surgery. In these cases, the vascular surgeon may need to perform an amputation as a last resort.